Dry Mouth Causes Bacterial Overgrowth and Recurring Oral Infections
Dry mouth, or xerostomia, reduces saliva, which is essential for maintaining oral health. A lack of saliva creates an environment that promotes bacterial overgrowth, leading to recurring oral infections. With decreased saliva, harmful bacteria thrive, disrupting the oral microbiome and increasing the risk of cavities and gum disease. This imbalance can also lead to bad breath. By exploring effective measures to manage dry mouth, you can better protect your oral health and prevent infections.
Key Takeaways
- Dry mouth reduces saliva, which is essential for maintaining oral pH balance and preventing bacterial overgrowth.
- A decrease in saliva’s antimicrobial properties allows harmful bacteria to proliferate, leading to oral infections.
- Insufficient saliva flow disrupts the oral microbiome, resulting in an imbalance favoring pathogenic bacteria.
- Symptoms of dry mouth can lead to increased tooth decay and gum disease due to higher acidity in the mouth.
- Regular hydration and good oral hygiene practices can help manage dry mouth and reduce the risk of infections.
Understanding Dry Mouth: Definition and Symptoms
Dry mouth, medically known as xerostomia, is a condition characterized by a decrease in saliva production, leading to discomfort and various oral health issues. You might experience symptoms such as a persistent dry feeling in your mouth, difficulty swallowing, and an increased thirst. Saliva reduction not only affects your ability to taste food but also disrupts the balance of your oral microbiome, which plays an essential role in maintaining oral health. A diminished saliva flow can encourage the growth of harmful bacteria and contribute to issues like bad breath and tooth decay. Understanding these symptoms is important for addressing dry mouth effectively and preventing further complications linked to oral health.
Common Causes of Dry Mouth
Dry mouth can stem from various factors that affect saliva production. You might experience it due to medication side effects, dehydration from illness, or even natural aging and hormonal changes. Understanding these common causes can help you address the issue and seek appropriate remedies.
Medication Side Effects
While many people may not realize it, certain medications can greatly contribute to dry mouth, a condition that can lead to discomfort and increase the risk of oral health issues. Common culprits include antihistamines, antidepressants, and blood pressure medications. When saliva production decreases, your mucosal defense weakens, making it easier for harmful bacteria to thrive. This bacterial overgrowth can result in recurring oral infections, such as cavities or gum disease. If you notice persistent dry mouth, it’s essential to consult your healthcare provider. They might adjust your medication or suggest alternatives that minimize side effects, helping you maintain your oral health and reduce the risk of complications associated with dry mouth. Taking action now can make a significant difference in your overall well-being.
Dehydration and Illness
When you’re dehydrated or battling an illness, your body’s ability to produce saliva can considerably diminish, leading to dry mouth. Dehydration often occurs due to insufficient fluid intake, excessive sweating, or illnesses that cause fever or vomiting. Conditions like the flu, cold, or infections can also disrupt normal bodily functions, including saliva production. In addition, certain gastrointestinal issues may exacerbate dehydration, compounding the problem. When you don’t have enough saliva, not only does your mouth feel uncomfortable, but you also increase your risk of dental problems and oral infections. Staying hydrated and addressing underlying health issues is essential for maintaining adequate saliva levels and preventing dry mouth. Prioritizing your health can help you avoid these complications.
Aging and Hormonal Changes
As you age, your body’s ability to produce saliva naturally declines, contributing to dry mouth. This condition can be exacerbated by hormonal changes, particularly in women during menopause. Several factors play a role in this process:
- Decreased Salivary Gland Function: Aging glands produce less saliva, leading to dryness.
- Medications: Many older adults take medications that list dry mouth as a side effect.
- Health Conditions: Chronic conditions like diabetes and autoimmune diseases can impact saliva production.
- Hormonal Shifts: Estrogen and progesterone fluctuations during menopause can decrease saliva flow.
Understanding these factors can help you manage dry mouth effectively, reducing the risk of bacterial overgrowth and oral infections. Prioritizing hydration and regular dental visits is essential for maintaining oral health.
The Role of Saliva in Oral Health
Saliva plays an essential role in maintaining your oral health by providing important protective functions. It helps regulate pH levels in your mouth, creating an environment that limits harmful bacterial growth. Understanding these functions highlights the significance of saliva in preventing issues like dry mouth and subsequent bacterial overgrowth.
Saliva’s Protective Functions
While you may not think about it often, saliva plays an essential role in maintaining oral health. Its protective functions are crucial for preventing infections and promoting overall well-being. Here are four key protective roles of saliva:
- Antimicrobial Action: Saliva contains enzymes and antibodies that inhibit the growth of harmful bacteria and fungi.
- Lubrication: It helps keep your mouth moist, facilitating speech and swallowing while reducing friction.
- Remineralization: Saliva contributes to the repair of tooth enamel by providing essential minerals like calcium and phosphate.
- pH Balance: It helps neutralize acids produced by bacteria, reducing the risk of tooth decay.
Ph Balance Regulation
Maintaining the right pH balance in your mouth is essential for preventing dental issues, and saliva plays a key role in this process. Saliva contains bicarbonate, which helps neutralize acids produced by bacteria and food. This buffering action protects your tooth enamel from erosion and decay. When your mouth is adequately hydrated, saliva flows freely, promoting a stable pH range that supports healthy oral flora. Conversely, a dry mouth can disrupt this balance, leading to an acidic environment conducive to dental problems. Regularly stimulating saliva production, through hydration or chewing sugar-free gum, can help maintain this balance. By prioritizing saliva’s role in pH regulation, you can considerably enhance your oral health and reduce the risk of infections.
Bacterial Growth Inhibition
When your mouth is adequately hydrated, it plays an essential role in inhibiting bacterial growth. Saliva contains various components that help maintain oral health, creating an environment less favorable for harmful bacteria. Here are four key ways saliva contributes to bacterial growth inhibition:
- Antibacterial Properties: Saliva includes enzymes like lysozyme that destroy bacterial cell walls.
- pH Balance: It helps maintain a neutral pH, reducing acidity that can promote bacterial proliferation.
- Flushing Effect: Saliva washes away food particles and debris, limiting the nutrients available for bacteria.
- Immunoglobulins: These proteins in saliva neutralize pathogens, providing an additional layer of defense.
Keeping your mouth hydrated is vital for these protective functions, promoting overall oral health.
How Dry Mouth Leads to Bacterial Overgrowth
Dry mouth, or xerostomia, can greatly alter the oral environment, creating conditions conducive to bacterial overgrowth. When saliva production decreases, you lose its natural protective properties, which include washing away food particles and neutralizing acids. This deficiency allows bacteria to thrive, as there’s less moisture to inhibit their growth. Without adequate saliva, the pH balance in your mouth shifts, further promoting harmful bacterial proliferation. Additionally, the reduced flow of saliva means fewer antimicrobial agents are present, weakening your mouth’s defenses. As a result, pathogenic bacteria can dominate, leading to an imbalance that exacerbates oral health issues. Recognizing these changes is essential for taking proactive steps to manage dry mouth and protect your oral health effectively.
The Impact of Bacterial Imbalance on Oral Health
Bacterial imbalance in your mouth can considerably impact your oral health, leading to a host of issues beyond just bad breath. When harmful bacteria outnumber beneficial ones, you might face several complications, including:
- Tooth decay – Increased acidity from harmful bacteria erodes enamel, promoting cavities.
- Gum disease – Imbalanced bacteria can cause inflammation, leading to gingivitis and periodontitis.
- Oral infections – A weakened immune response can make you more susceptible to infections like thrush.
- Halitosis – The proliferation of certain bacteria can lead to persistent bad breath.
Maintaining a balanced oral microbiome is essential for preventing these issues and promoting overall oral health. Regular dental check-ups and proper hygiene practices can help you keep bacterial imbalance in check.
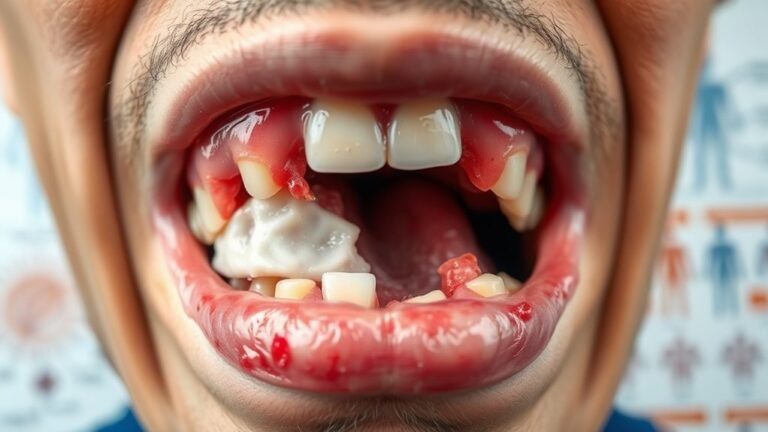
Recognizing the Signs of Oral Infections
How can you tell if you’re experiencing an oral infection? Look for common signs such as persistent pain, swelling, or redness in your gums or mouth. You might also notice a bad taste or foul breath that doesn’t go away. If you see white patches or sores on your tongue or inside your cheeks, these can indicate an infection. Increased sensitivity to hot or cold foods and difficulty swallowing are also red flags. Additionally, if you experience fever or swollen lymph nodes, it’s essential to consult a healthcare professional. Recognizing these symptoms early can help you address the infection promptly and prevent further complications. Stay vigilant about your oral health to maintain overall well-being.
Preventive Measures for Managing Dry Mouth
When managing dry mouth, it is crucial to adopt preventive measures that can considerably alleviate symptoms and improve your oral health. Here are four effective strategies you can implement:
- Stay Hydrated: Drink plenty of water throughout the day to keep your mouth moist and support saliva production.
- Chew Sugar-Free Gum: This stimulates saliva flow, helping to combat dryness and maintain oral moisture.
- Use a Humidifier: Adding moisture to the air while you sleep can prevent nighttime dryness, promoting a more comfortable environment.
- Avoid Certain Foods: Limit caffeine, alcohol, and spicy foods, as these can exacerbate dry mouth symptoms.
Treatment Options for Dry Mouth and Related Infections
To effectively manage dry mouth and its associated infections, it is essential to explore various treatment options tailored to your needs. Here are some effective strategies:
| Treatment Option | Description | Effectiveness |
|---|---|---|
| Saliva Substitutes | Over-the-counter gels or sprays | Quick relief |
| Hydration | Drinking water or herbal teas | Ongoing support |
| Prescription Medications | Salivary stimulants like pilocarpine | Variable effectiveness |
| Mouth Rinses | Antimicrobial or saline rinses | Infection prevention |
| Sugar-Free Lozenges | Stimulate saliva production | Immediate relief |
Maintaining a Healthy Oral Microbiome
Maintaining a healthy oral microbiome is essential for preventing bacterial overgrowth and supporting overall oral health. You can take proactive steps to nurture your oral environment and reduce the risk of infections by following these guidelines:
- Stay Hydrated: Drink plenty of water throughout the day to keep your mouth moist and help wash away bacteria.
- Practice Good Oral Hygiene: Brush your teeth twice daily and floss regularly to remove plaque and food particles.
- Limit Sugar Intake: Reduce sugary foods and drinks that can fuel harmful bacteria growth.
- Use Probiotics: Consider adding probiotic-rich foods or supplements to support beneficial bacteria in your mouth.
Frequently Asked Questions
Can Dry Mouth Affect Taste Perception?
Yes, dry mouth can considerably affect your taste perception. When saliva production decreases, taste buds may struggle to function properly, leading to altered or diminished taste experiences, making food less enjoyable or flavorful for you.
Are Certain Medications More Likely to Cause Dry Mouth?
Yes, certain medications, like antihistamines, antidepressants, and blood pressure drugs, can cause dry mouth. If you’re experiencing this side effect, consult your doctor to explore alternatives or solutions to help alleviate your symptoms effectively.
How Does Dehydration Contribute to Dry Mouth?
Think of your mouth as a garden; without water, it wilts. Dehydration reduces saliva production, leading to dry mouth, which can affect your oral health and comfort. Staying hydrated keeps your mouth flourishing.
Can Diet Influence Dry Mouth Severity?
Yes, your diet can influence dry mouth severity. Consuming salty, sugary, or caffeinated foods and drinks can exacerbate dryness, while hydrating foods like fruits and vegetables, along with plenty of water, can help alleviate symptoms.
Is Dry Mouth More Common in Specific Age Groups?
Yes, dry mouth’s definitely more prevalent in older adults. As you age, saliva production often decreases, leading to discomfort and potential complications. Staying hydrated and consulting a healthcare professional can help manage this issue.
Conclusion
In conclusion, understanding and addressing dry mouth is essential for maintaining oral health. Just as a garden needs water to flourish, your mouth relies on saliva to keep harmful bacteria at bay. By recognizing the signs and implementing preventive measures, you can combat bacterial overgrowth and reduce the risk of recurring infections. Don’t neglect your oral hygiene; take proactive steps to guarantee your mouth stays healthy and your smile remains bright.