How Do Immune System Deficiencies Contribute to Recurring Oral Infections
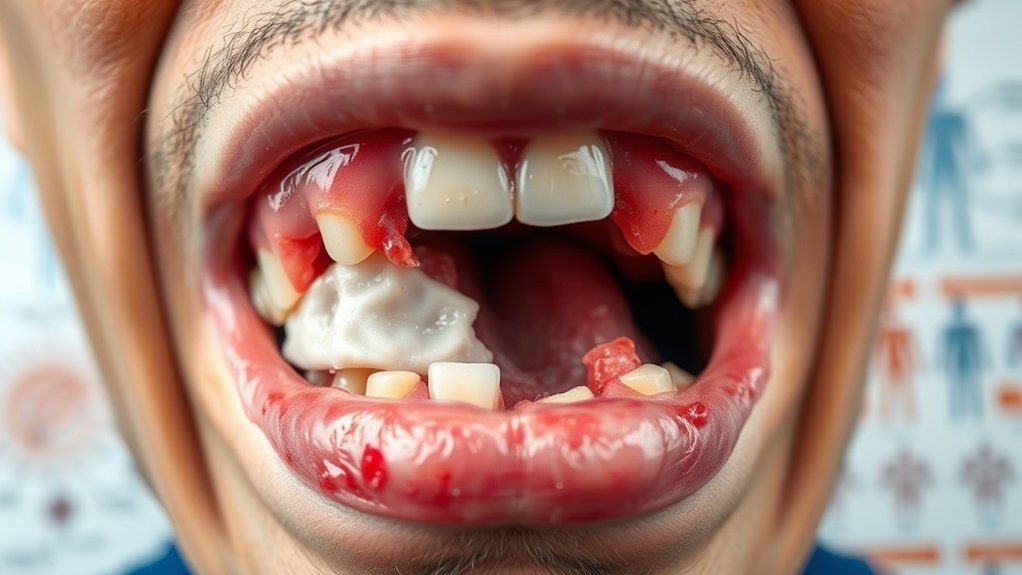
Immune system deficiencies greatly increase your risk of recurring oral infections. Conditions like IgA deficiency impair mucosal immunity, making you more susceptible to gingivitis and periodontitis. If you have T-cell deficiency, you’ll struggle against opportunistic infections in the oral cavity. Additionally, neutrophil dysfunction hampers your body’s ability to combat bacteria effectively. Recognizing and addressing these deficiencies is crucial for oral health. There are more strategies to enhance your immune function and protect your oral environment.
Key Takeaways
- Immune deficiencies, such as IgA deficiency, reduce mucosal immunity, increasing the risk of conditions like gingivitis and periodontitis.
- T-cell deficiencies can lead to opportunistic infections in the oral cavity, making individuals more prone to recurring infections.
- Neutrophil dysfunction impairs the body’s ability to combat bacterial infections, heightening susceptibility to oral health issues.
- Autoimmune disorders can disrupt normal immune responses, exacerbating inflammation and increasing the likelihood of oral infections.
- Nutritional deficiencies weaken immune function, contributing to increased susceptibility to infections in the oral cavity.
Understanding the Immune System’s Role in Oral Health
Understanding the immune system’s role in oral health is essential, especially since a robust immune response can prevent oral infections. Central to this is mucosal immunity, which primarily involves the oral mucosa. This specialized immune response acts as a frontline defense against pathogens entering through oral tissues. Secretory immunoglobulin A (sIgA) plays a pivotal role in mucosal immunity by neutralizing bacteria and viruses, preventing their adherence to mucosal surfaces. Additionally, dendritic cells in the oral mucosa capture antigens and activate T-cells, leading to a targeted immune response. This complex interplay guarantees that the oral cavity remains resilient against infections. If mucosal immunity is compromised, the risk of oral infections increases, emphasizing the need for a well-functioning immune system in maintaining oral health.
Common Immune System Deficiencies and Their Impact
Compromised mucosal immunity can lead to various immune system deficiencies that greatly impact oral health. Understanding these immune deficiencies is essential for preventing recurring oral infections. Here are three common deficiencies you should be aware of:
- IgA Deficiency: This deficiency reduces mucosal immunity, increasing susceptibility to infections like gingivitis and periodontitis.
- T-Cell Deficiency: T-cells play a significant role in regulating immune responses; their deficiency can lead to opportunistic infections in the oral cavity.
- Neutrophil Dysfunction: Impaired neutrophil function hampers the ability to fight off bacterial infections, leading to persistent oral issues.
Recognizing how these immune deficiencies affect your oral health can empower you to take preventive measures and seek appropriate treatments.
How Autoimmune Disorders Affect Oral Infections
Autoimmune disorders, such as lupus and rheumatoid arthritis, can greatly compromise your oral health by triggering inflammation and altering immune responses. You may notice symptoms like dry mouth or gum disease, which can exacerbate existing oral infections. Understanding the types of autoimmune disorders and their management strategies is essential for mitigating these effects and maintaining oral hygiene.
Types of Autoimmune Disorders
How do various types of autoimmune disorders influence the risk and severity of oral infections? Autoimmune disorders can greatly compromise your immune response, making you more susceptible to recurrent oral infections. Here are three common types that impact oral health:
- Sjogren’s Syndrome: This disorder reduces saliva production, leading to dry mouth, which fosters bacterial growth and increases the risk of cavities and gum disease.
- Lupus: The systemic inflammation from lupus can cause painful ulcers in the mouth, exacerbating oral infections.
- Rheumatoid Arthritis: This condition can lead to gum inflammation, and the medications used may further weaken your immune system, heightening infection risks.
Understanding these autoimmune disorders is essential for managing oral health effectively.
Symptoms Impacting Oral Health
While many people may underestimate the connection between systemic health and oral well-being, symptoms from autoimmune disorders can greatly impact oral infections. Conditions like Sjögren’s syndrome lead to reduced saliva production, causing dry mouth that fosters bacterial growth and increases the risk of oral infections. Similarly, lupus and rheumatoid arthritis can trigger inflammation, affecting the gums and making them more susceptible to infection. You might also experience ulcers or lesions, which can serve as entry points for pathogens. These symptoms not only compromise your oral health but can also exacerbate the autoimmune condition itself, creating a vicious cycle. Recognizing these connections is vital for understanding how your overall health directly influences your oral infections.
Treatment and Management Strategies
Understanding the interplay between autoimmune disorders and oral health is essential for managing oral infections effectively. Autoimmune conditions can lead to a bacterial imbalance in your oral microbiome, increasing susceptibility to infections. Here are three strategies to take into account:
- Regular Dental Check-ups: Routine visits to your dentist can help identify early signs of infections, allowing for prompt intervention.
- Antibiotic Therapy: In some cases, targeted antibiotics may be necessary to restore balance in the oral flora, particularly during flare-ups.
- Dietary Adjustments: Incorporating anti-inflammatory foods can support your immune system and help mitigate the effects of autoimmune disorders on your oral health.
The Connection Between Stress and Immune Function
Stress considerably impacts immune function, as prolonged psychological strain can lead to a cascade of physiological responses that weaken your body’s defenses. When you experience stress, your body produces increased levels of cortisol, which, while beneficial in short bursts, can suppress immune responses over time. This suppression makes you more susceptible to infections, including oral ones. Moreover, chronic stress can contribute to systemic illness by disrupting the balance of cytokines, essential in regulating inflammation and immune responses. If you’re under constant stress, your immune system may fail to respond adequately to pathogens, leading to recurring oral infections. Understanding this connection emphasizes the importance of stress management in maintaining a robust immune system and preventing complications.
Nutritional Deficiencies and Their Effects on Immunity
Chronic stress compromises your immune system, but it’s not the only factor that can lead to vulnerabilities. Nutritional deficiencies can severely impact immune function, resulting in immunosuppression. Without essential nutrients, your body struggles to fend off infections, including recurrent oral issues. Consider these important nutrients:
- Vitamin C: Key for collagen synthesis and immune cell function; deficiency can lead to delayed healing.
- Zinc: Fundamental for immune cell development; insufficient levels can decrease your body’s response to pathogens.
- Vitamin D: Plays a role in immune regulation; low levels are linked to increased susceptibility to infections.
Addressing these nutritional gaps is essential for maintaining a robust immune system and preventing recurring oral infections.
Strategies for Strengthening the Immune System
To effectively strengthen your immune system, focus on optimizing your nutrition and maintaining a regular exercise routine. A balanced diet rich in vitamins and minerals provides essential support for immune function, while consistent physical activity enhances circulation and reduces inflammation. Evaluating these two components can greatly improve your overall immunity and resilience against infections.
Nutrition and Diet
While maintaining a balanced diet is often overlooked, it plays an essential role in fortifying your immune system against infections, including those affecting the oral cavity. A nutritious diet can help combat chronic infections by providing the necessary vitamins and minerals that enhance immune function. Consider these key strategies:
- Incorporate Antioxidants: Foods rich in vitamins C and E, like citrus fruits and nuts, help protect cells from damage.
- Boost Probiotics: Fermented foods like yogurt and kefir support gut health, vital for immune response.
- Prioritize Zinc: Including zinc-rich foods, such as oysters and legumes, can improve your body’s ability to fight off infections.
Regular Exercise Routine
Engaging in a regular exercise routine not only enhances physical fitness but also plays a significant role in strengthening your immune system. When you exercise, circulation improves, allowing immune cells to travel more efficiently throughout your body. This increased mobility helps your immune system detect and combat pathogens more effectively, reducing the likelihood of infections, including oral ones. Additionally, regular exercise can help manage stress, a known suppressor of immune function. Importantly, physical activity can influence the composition of biofilm in your oral cavity, promoting a healthier microbial balance. This balance is essential for preventing the overgrowth of harmful bacteria that can lead to oral infections. As a result, incorporating consistent exercise into your lifestyle is critical for maintaining a robust immune response.
Treatment Options for Recurring Oral Infections
When dealing with recurring oral infections, it’s important to explore various treatment options that can effectively manage symptoms and address underlying causes. Prioritizing your dental health is vital in this process. Here are three treatment options to keep in mind:
- Antibiotics: These can target bacterial infections, helping to reduce inflammation and promote healing. Your dentist may prescribe a specific antibiotic based on culture results.
- Antifungal Medications: If oral thrush is a recurring issue, antifungal treatments can help eliminate yeast overgrowth.
- Oral Hygiene Practices: Improving your daily oral hygiene, such as regular brushing and flossing, can prevent infections from developing by maintaining a healthy oral environment.
Frequently Asked Questions
Can Allergies Affect Oral Health and Immune Function?
Yes, allergies can negatively impact your oral health and immune function. When allergic reactions occur, inflammation increases, potentially leading to oral discomfort, which may compromise your immune response and heighten susceptibility to infections.
How Does Age Influence Immune System Effectiveness?
As you age, your immune system weakens, much like a fading warrior. It struggles to fend off infections, leading to increased vulnerability. Cellular response slows, and inflammation can rise, leaving you more susceptible to oral health issues.
Are There Specific Medications That Weaken the Immune System?
Yes, certain medications like corticosteroids, chemotherapy drugs, and immunosuppressants can weaken your immune system. They reduce your body’s ability to fight infections, making you more susceptible to illnesses and complications from infections.
Can Oral Hygiene Practices Boost Immune Health?
Yes, maintaining good oral hygiene practices, like regular brushing and flossing, can enhance your immune health. These practices reduce harmful bacteria, prevent infections, and support your body’s overall defense mechanisms against pathogens.
Is There a Link Between Gut Health and Oral Infections?
Absolutely, gut health acts like a well-tuned orchestra, influencing oral infections. A balanced microbiome can enhance your immune response, preventing harmful bacteria in the mouth from thriving and reducing the likelihood of recurring infections.
Conclusion
In conclusion, immune system deficiencies play an essential role in the frequency and severity of oral infections. As the saying goes, “an ounce of prevention is worth a pound of cure.” Strengthening your immune system through proper nutrition, stress management, and understanding autoimmune impacts can greatly reduce the risk of recurring infections. By addressing these factors proactively, you not only enhance your overall health but also safeguard your oral well-being against persistent threats.