Can Dental Implants Affect Oral Bacterial Balance and Cause Infections
Dental implants can indeed affect your oral bacterial balance. Their surfaces may promote bacterial colonization, potentially leading to complications like peri-implantitis if not maintained properly. The materials used and your oral hygiene habits greatly influence this balance. If harmful bacteria flourish, you could face inflammation and infection risks. Knowing how to care for your implants and maintain a healthy mouth is essential. Learn about preventive measures and the long-term implications to safeguard your oral health.
Key Takeaways
- Dental implants can alter the balance of oral bacteria, potentially leading to an increase in pathogenic species and biofilm formation.
- The surface characteristics of implants influence bacterial colonization, affecting the microbial community around the implant site.
- Poor oral hygiene post-implantation increases the risk of peri-implantitis, an inflammation that can compromise implant stability.
- Regular dental check-ups and proper hygiene are essential to prevent infections and monitor changes in the oral microbiome.
- Dietary choices and antimicrobial mouthwashes can help maintain a healthy bacterial balance, supporting implant success and reducing infection risks.
Understanding Dental Implants and Their Function
Although dental implants have become a popular solution for missing teeth, understanding how they function is fundamental for appreciating their role in oral health. Dental implants consist of titanium posts surgically placed into the jawbone, where they fuse with the bone through a process called osseointegration. This stability allows them to act as strong anchors for replacement teeth. The biocompatibility of titanium minimizes the risk of rejection, promoting a secure fit. Additionally, dental implants help preserve jawbone density by stimulating bone growth, preventing the deterioration that often follows tooth loss. Proper placement and maintenance of dental implants are vital for long-term success, ensuring they effectively restore both function and aesthetics while supporting overall oral health.
The Role of Oral Bacteria in Dental Health
Dental health is intricately linked to the balance of oral bacteria, which play a significant role in both maintaining and disrupting oral ecosystems. A diverse array of bacteria exists in your mouth, and a healthy oral bacterial balance contributes to processes like digestion and immune defense. When this balance is disrupted, harmful bacteria can proliferate, leading to conditions such as gingivitis and periodontitis. Research shows that an unhealthy bacterial environment can also contribute to systemic issues, affecting overall health. Maintaining oral hygiene, including regular brushing and flossing, is essential to support a healthy microbial community. By doing so, you not only protect your teeth and gums but also promote a balanced oral microbiome, which is vital for lasting dental health.
How Dental Implants Interact With Oral Microflora
Dental implants greatly influence the oral microflora due to their unique surface characteristics, which can affect bacterial colonization. You’ll find that the dynamics of bacterial attachment and growth on these surfaces play an essential role in shaping the surrounding microbial community. Additionally, the presence of implants can modulate the immune response, impacting how your body interacts with these microorganisms.
Implant Surface Characteristics
Implant surface characteristics play an essential role in how dental implants interact with oral microflora. The texture and chemical composition of implant surfaces influence bacterial adhesion and biofilm formation. These factors can either promote or inhibit the growth of specific bacteria, ultimately affecting oral health.
| Surface Type | Bacterial Adhesion |
|---|---|
| Smooth | Lower adhesion rates |
| Rough | Higher adhesion rates |
| Coated | Varies with coating type |
| Titanium alloy | Moderate adhesion |
Understanding these interactions helps in selecting appropriate implant surfaces that minimize infection risks and maintain a balanced oral microflora. By choosing the right implant surface, you can enhance the longevity of your dental implants and promote better oral health outcomes.
Bacterial Colonization Dynamics
When considering how implants interact with oral microflora, it’s vital to understand the dynamics of bacterial colonization. Dental implants provide a surface for bacterial adhesion, which can lead to changes in the surrounding microbial community. The roughness and texture of the implant surface influence how bacteria attach, often resulting in a biofilm formation that can harbor pathogenic species. Research shows that certain bacteria thrive on implant surfaces more than natural teeth, leading to an imbalance in the oral ecosystem. This imbalance can contribute to peri-implantitis, a condition characterized by inflammation and infection. Consequently, understanding bacterial colonization dynamics on implants is fundamental for preventing complications and maintaining oral health post-implantation. Monitoring these dynamics can help in developing better preventive strategies.
Immune Response Modulation
While you might expect that the introduction of foreign materials in the oral cavity would provoke a uniform immune response, the reality is much more complex. Dental implants can modulate the immune response, creating a unique environment for oral microflora. This modulation can influence the balance of bacterial populations, potentially leading to conditions like peri-implantitis. In this scenario, the immune system may overreact to the presence of implants, fostering an inflammatory response that disrupts bacterial equilibrium. Conversely, a compromised immune response may allow pathogenic bacteria to thrive, exacerbating the risk of infection. Understanding these dynamics is essential for managing oral health post-implantation, ensuring that you maintain a stable balance of beneficial bacteria while preventing complications.
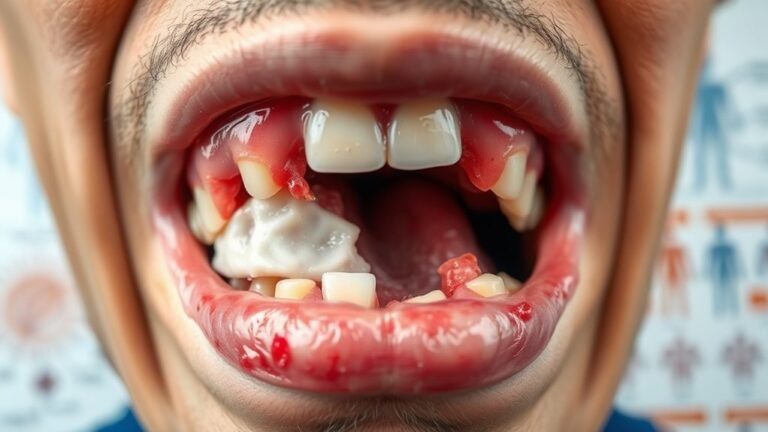
Potential Risks of Infection After Implant Surgery
Although dental implants are a popular solution for tooth loss, they come with potential risks, particularly regarding infection following surgery. A bacterial infection can occur at the implant site, leading to complications such as peri-implantitis, which involves inflammation of the surrounding tissue. This condition can compromise the stability of the implant and ultimately result in implant failure. Studies indicate that factors like surgical technique, patient hygiene, and pre-existing health conditions influence infection risk. It’s imperative to follow post-operative care guidelines diligently, as this helps mitigate the chances of bacterial colonization. Regular dental check-ups are also essential for monitoring your oral health and addressing any signs of infection early, ensuring the long-term success of your dental implant.
Factors Influencing the Balance of Oral Bacteria
The composition of the materials used in dental implants greatly affects the balance of oral bacteria. When you maintain proper oral hygiene practices, you can further influence this microbial environment, reducing the risk of complications. Understanding these factors is essential for achieving long-term success with dental implants.
Implant Material Composition
As dental implants become increasingly prevalent in restorative dentistry, understanding how their material composition affects the balance of oral bacteria is essential. Different implant materials can alter the oral microbiome, potentially leading to infections. Titanium, for example, is widely used for its biocompatibility. However, newer materials like zirconia are being explored for their potential benefits in reducing bacterial adhesion.
| Implant Material | Bacterial Adhesion |
|---|---|
| Titanium | Moderate |
| Zirconia | Low |
| Stainless Steel | High |
| Polyetheretherketone | Low |
| Ceramic | Very Low |
Your choice in implant materials can influence not just the success of the procedure but also your long-term oral health. Understanding these implications is vital.
Oral Hygiene Practices
Effective oral hygiene practices are essential for maintaining a balanced oral microbiome, particularly in individuals with dental implants. Daily brushing and flossing help remove plaque, a key contributor to bacterial imbalance. Studies show that neglecting these practices can lead to an overgrowth of harmful bacteria, increasing the risk of peri-implantitis and infections. Using antimicrobial mouthwashes can further support your efforts by targeting pathogenic bacteria without disrupting beneficial species. Regular dental check-ups allow for professional cleanings and early identification of potential issues, ensuring your oral microbiome remains healthy. Additionally, a balanced diet rich in nutrients can promote the growth of beneficial bacteria, enhancing your overall oral health. Prioritizing these practices can greatly influence your oral microbiome and implant longevity.
Preventive Measures to Maintain Oral Health With Implants
While dental implants can greatly enhance your oral function and aesthetics, maintaining oral health around these restorations requires diligent preventive measures. Effective implant maintenance is vital to prevent infections and guarantee longevity. Here are four essential steps you can take:
- Regular brushing and flossing: Clean around implants daily to remove plaque and food particles.
- Routine dental check-ups: Schedule visits every six months for professional cleaning and monitoring of implant health.
- Use antimicrobial mouthwash: Incorporate a mouthwash that targets bacteria to reduce the risk of infections.
- Avoid tobacco products: Smoking can impair healing and increase the likelihood of complications around implants.
Long-term Implications of Dental Implants on Oral Microbial Balance
Understanding the long-term implications of dental implants on oral microbial balance is vital for maintaining overall oral health. Research shows that dental implants can alter the composition of oral biofilm, promoting the growth of pathogenic bacteria. This shift may lead to peri-implantitis, a condition characterized by inflammation and potential bone loss around the implant. Over time, the presence of implants may create a unique environment that fosters a microbial community distinct from natural teeth. Regular monitoring of biofilm formation and diligent oral hygiene practices are important to mitigate risks. By being proactive, you can greatly reduce the likelihood of infections and guarantee your dental implants contribute positively to your oral health in the long run.
Frequently Asked Questions
Can Dental Implants Cause Allergic Reactions in Some Patients?
Yes, dental implants can cause allergic reactions in some patients. These reactions often stem from materials like titanium or certain alloys. If you experience unusual symptoms post-implant, consult your dentist for evaluation and potential alternatives.
How Do Smoking and Tobacco Use Impact Implant Success?
Smoking and tobacco use sabotage implant success like a storm erodes a shoreline. They impair blood flow, delay healing, and increase infection risk, ultimately leading to higher failure rates in dental implants. Quitting improves outcomes considerably.
Are There Specific Bacteria That Thrive Around Dental Implants?
Yes, specific bacteria like Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans often thrive around dental implants. Their presence can lead to peri-implantitis, which negatively impacts implant success and overall oral health if not properly managed.
What Is the Average Recovery Time Post-Implant Surgery?
You’ll generally recover from implant surgery in about three to six months. Isn’t it fascinating how your body heals? Factors like overall health and implant location can influence this timeline, so consult your dentist for personalized guidance.
Can Dental Implants Affect Taste Perception or Oral Sensations?
Dental implants can temporarily affect taste perception and oral sensations due to changes in oral structure. Most patients report improvements over time, but individual experiences vary, so discussing concerns with your dentist’s essential for tailored advice.
Conclusion
In summary, while dental implants can enhance your smile and functionality, they may also disrupt your oral bacterial balance, potentially leading to infections. For instance, a study involving patients with implants showed that those who didn’t maintain rigorous oral hygiene experienced higher rates of peri-implantitis. As a result, it’s essential to adopt preventive measures, such as regular dental check-ups and proper cleaning routines, to minimize risks and guarantee long-term oral health after implant placement.